PERICORONITIS SYMPTOMS AND TREATMENT FOR BETTER ORAL HEALTH
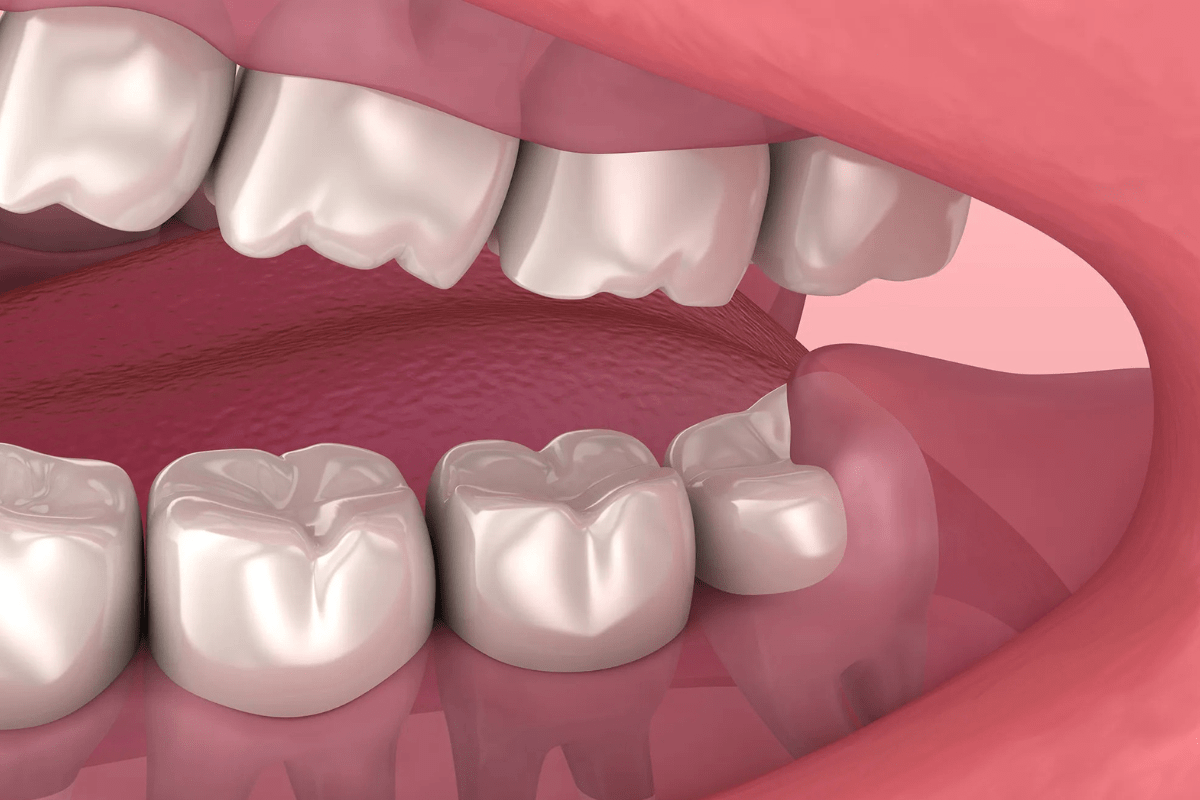
Pericoronitis is a condition that occurs when wisdom teeth don’t have enough space to fully emerge from the gums. If they only partially break through, inflammation and swelling can develop around the tooth, causing discomfort and further complications. If the wisdom teeth are partially erupted, gum flaps can form, creating spaces where food particles can become trapped. Bacteria can then build up, leading to infection.
Key Facts:
- Wisdom teeth typically emerge in late adolescence.
- Pericoronitis can be acute (short-term) or chronic (long-term).
- It most commonly affects individuals between the ages of 20 and 40.
WHAT IS PERICORONITIS?
Pericoronitis is the swelling of the gum tissue around wisdom teeth, also known as third molars. These are the last adult teeth to emerge, usually in your late teens or early twenties. Pericoronitis develops when a wisdom tooth is only partially erupted or trapped beneath the gum, causing irritation and infection. It is more common in the lower wisdom teeth but can also affect the upper ones.
IMPACT ON ORAL HEALTH:
An affected wisdom tooth may lead to the development of a gum flap or operculum, which partially covers the tooth crown. Food, bacteria, and debris can become trapped under the operculum, creating an environment for infection.
WHO IS AFFECTED?
Pericoronitis is common in people with wisdom teeth, particularly those aged 20 to 29. Both men and women are affected equally by the condition.
SYMPTOMS:
Symptoms vary depending on whether the condition is acute or chronic.
Acute Symptoms:
- Intense pain near the back teeth
- Swelling of the gum tissue
- Pain when swallowing
- Pus discharge
- Lockjaw (trismus)
Chronic Symptoms:
- Bad breath
- A bad taste in the mouth
- Mild pain lasting up to two days
CAUSES AND RISK FACTORS:
Pericoronitis usually happens when a wisdom tooth partially emerges and bacteria accumulate in the soft tissue around it, causing inflammation. Several factors can increase the risk of developing pericoronitis:
- Age (typically between 20 and 29)
- Wisdom teeth that are impacted or haven’t fully erupted
- Poor oral hygiene
- Excessive gum tissue
- Emotional stress, fatigue, or pregnancy
Overall, health is not a significant factor in the development of pericoronitis.
DIAGNOSIS:
A dentist will examine the wisdom teeth to assess their position and determine if they are partially impacted. X-rays may be used periodically to monitor the eruption of the wisdom teeth. The dentist will also check for signs of infection, swelling, or gum flaps around the affected tooth.
TREATMENT:
WHAT IS THE BEST WAY TO TREAT PERICORONITIS?
Pericoronitis treatment differs for each patient. In the event of inflammation, your dentist may suggest cleaning the area with pericoronitis mouthwash, antibiotics, removal of pericoronitis, and wisdom teeth extraction.
Dental cleaning:
The dentist will rinse the affected area to eliminate all food debris, bacteria, or other particles. They might also prescribe medicines, such as antibacterial mouthwash or antibiotics.
Antibiotics:
Oral antibiotics can help eliminate an infection called pericoronitis. Be sure to take all medicines exactly as instructed by your doctor.
Pericoronitis mouthwash:
Your dentist might suggest using a prescribed chlorhexidine mouthwash as a topical antiseptic. This assists in eliminating harmful bacteria that reside in your mouth.
Chlorhexidine rinses might experience short-term negative side effects, including an alteration in taste or staining of the teeth. These effects are usually temporary. Follow the instructions given by the dentist.
Pericoronitis removal surgery:
Often, your dentist will suggest removing your gum flap (operculum). This will require a quick oral surgical procedure. Anesthesia is possible but typically not required. Your doctor will often complete the procedure using local anesthesia in under one hour.
Wisdom tooth removal surgery:
If your wisdom tooth is causing pericoronitis and other issues, wisdom tooth removal might be necessary. A periodontist or oral surgeon can perform this procedure without or with sedation.
Dental cleaning:
While it is important to visit your dentist or dental surgeon to discuss a personalized treatment, they could suggest home remedies. They should be done alongside, but not instead of, professional treatment. Home solutions comprise:
- Prescription painkillers available on the market
- Warm salt-water rinses
- oral water irrigation
- Good oral hygiene includes flossing and brushing
Avoid applying hot compresses. Consult a doctor if you suffer from an illness causing a fever.
COMPLICATIONS:
If untreated, pericoronitis can lead to complications, such as:
- Infection Spread: The infection may spread, causing swelling and discomfort in the neck and head.
- Trismus (Lockjaw): Difficulty opening the mouth or biting down.
- Serious Infections: Rarely untreated pericoronitis can lead to Ludwig’s angina, a life-threatening infection beneath the tongue and jaw, or sepsis, which can be fatal.
PROGNOSIS:
If treated early, most people recover from pericoronitis within a week or two. Severe cases may require surgery, such as removal of the gum flap or wisdom teeth. After surgery, some discomfort, jaw stiffness, and mild swelling may persist for up to two weeks.
IS PERICORONITIS SERIOUS?
If left untreated, pericoronitis can develop into an abscess, and the infection may spread to other body areas. In rare cases, it can become life-threatening. However, with prompt treatment, most cases are not serious, and patients recover fully.
LIVING WITH PERICORONITIS:
If you experience symptoms of pericoronitis, such as pain, swelling, or fever, consult your dentist immediately. Early intervention can prevent complications and provide relief. Depending on the severity of your condition, your dentist may recommend antibiotics and further treatment options.
PREVENTION:
A good oral hygiene regimen can prevent the pericoronitis infection from developing. Some steps people can adopt to lower the risk of developing pericoronitis include:
- Proper oral hygiene: Additional tooth cleaning to remove food debris and bacterial matter will aid.
- A regular visit to the dentist: Regular visits can help the dentist spot any indications or issues associated with pericoronitis, thereby increasing the chances of addressing them in the early stages.
- Making a pre-emptive call to the dentist whenever a person is concerned about pericoronitis’s development is suggested.
FINAL WORDS:
Pericoronitis is not known to cause long-term consequences. If the wisdom tooth completely develops or is removed, pericoronitis is unlikely to recur in the region. If a tooth has to be removed, the patient can usually expect complete recovery in about two weeks. After recovery, patients could feel:
- Jaw stiffness
- A mildly unpleasant taste in the mouth
- Swelling
- Pain
- A tingling or numbness in the face and mouth (less frequent)
Follow all instructions for aftercare, which is vital. In the event of severe or throbbing pain or fever, consult the dentist of one’s choice. The most important aspect to consider when treating pericoronitis is ensuring that the patients receive the proper treatment to treat the pain-inducing condition quickly. Contact a dentist immediately in case of any symptom.